The third session of the American Hospital Association’s Affinity Forum Series, hosted in partnership with StaffGarden by Ascend Learning, tackled one of the most pressing challenges in healthcare today: data fragmentation.
From siloed systems to poor strategic alignment, these barriers prevent organizations from making timely, informed decisions that impact patient care and workforce development.
Carol Gabala, MSN, RN, NPD-BC, System Director of Nursing Practice Excellence at Bon Secours Mercy Health shares one health system’s journey through data integration and the insights unlocked by data-driven decision-making capabilities.
The session, led by AHA’s Elisa Arespacochaga and featuring StaffGarden by Ascend Learning’s Vice President of Healthcare Workforce Solutions, Larissa Africa, MBA, RN, CENP, FAONL, FAAN explored how strategic workforce intelligence, powered by data integrations and smart governance, can turn challenges into opportunities.
Watch the full AHA Affinity Forum Session Three recording now.
Many healthcare organizations operate with disconnected technologies and processes. This fragmentation creates:
· Inconsistent metrics and reporting, limiting performance insights.
· Missed opportunities for upskilling and career development.
· Inefficient resource allocation, leading to delays in care.
· Reactive processes, rather than proactive workforce planning.
These issues impact patient outcomes and staff engagement, as well as create operational burdens.
Africa noted that healthcare organizations often operate within siloed systems, using a plethora of technologies and processes to manage the delivery of care. Leaders and those who need access to quality and workforce data are often overwhelmed when determining which system holds what data, whether that data is valid, and if it’s actionable in a timely manner.
As a result of data fragmentation, healthcare systems experience:
• Missed opportunities for upskilling
• Inefficient resource allocation
• Poor strategic alignment
Gabala shared that “Bon Secours Mercy Health is an international healthcare system with a geographically diverse and dispersed workforce, which creates unique challenges as we try to provide excellence across the system.”
She acknowledged that prior to implementing StaffGarden, BonSecours Mercy Health “experienced missed opportunities for upskilling staff, not recognizing clinical excellence, and inconsistent, reactive processes rather than proactive ones regarding the data we have.”
Bon Secours Mercy Health thus endured “a lot of manual processes— trying to figure out how to get the right care to the right patient at the right time— because maybe we didn’t even have that in a database. It was all on paper in somebody’s folder somewhere,” Gabala noted.
The forum emphasized that solving fragmentation requires more than technology—it demands a cultural and strategic shift. Integration unlocks:
· Centralized, real-time data accessible across the organization.
· Cross-functional insights that connect clinical performance, engagement, and development.
· Predictive and prescriptive analytics to anticipate staffing needs and reduce turnover risk.
This approach enables organizations to move from anecdotal decision-making to data-driven strategies that align with business goals.
“Through implementing digital competency tools and a digital clinical ladder, we’re creating standardization and aligning workforce development with strategic needs,” Gabala shared. “Data integration is really gonna help us tell our story and help us to predict what we need for the future to care for these patients so that we can make more proactive decisions.”
The panelists discussed the implementation of digital competency platforms and clinical ladders integrated with HR systems.These tools provide the ability to:
· Standardize competency tracking across diverse locations.
· Create transparent career pathways for nurses and other roles.
· Support competency-based onboarding, reducing orientation costs.
· Enable predictive modeling for turnover and advancement readiness.
The result: better talent decisions, proactive workforce planning, and measurable ROI through improved retention and patient outcomes.
“Our competency platform has been a game-changer,” Gabala shared. “Orientation is a very expensive timeframe within a nurse’s career.Having real-time data helping us monitor orientation progress, intervene early, and reduce costs has been huge. Consolidated dashboards give managers visibility into turnover and engagement that is up-to-date and accurate rather than relying on an anecdotal history.”
“Having a clinical ladder is always a good strategy for nurse recruitment, because it speaks to the organization’s investment in their nurses. It really does help us to be able to make better decisions, that can help us with promotion and succession planning,” Gabala noted.
Gabala then shared how the clinical ladder and competency data is already providing actionable insights to the leadership team to support the nursing workforce across the organization, for new and experienced nurses alike.
Bon Secours Mercy Health is now able to reimagine mentorship and coaching to better fit the needs of each unit systemwide. For example, “we’re using the system to create dyad and triad models of small groups to coach and mentor new nurses based on competency. There’s no paper that got left in a car or sitting at home— anybody can go in and look at the documentation to seethe opportunities, pull certain individuals together into a strong team faster to help nurses get to where they need to be to provide safe, competent care.”
Bon Secours Mercy Health is “beginning to explore predictive modeling for turnover risk and readiness for advancement so that we can predict future staffing needs based on ladder progression and competency,” Gabala added, a testament to the strategic workforce insights made possible by data-driven digital platforms like StaffGarden.
Integrating these tools with HR systems allows Bon SecoursMercy Health to more accurately track KPIs and measure ROI in a timely manner. Rather than being an expense to healthcare systems that lacks visibility into outcomes, “now we can see how these programs impact turnover, patient outcomes, and strategic goals. This duality— growing nurses and improving patient care—really supports our ministry goals as well,” Gabala added.
While clinical ladders traditionally focus on nursing, organizations are now extending these programs to other roles such as patient care technicians and medical assistants. This expansion fosters internal mobility and helps employees visualize long-term career opportunities, strengthening engagement and retention across the workforce.
“[Bon Secours Mercy Health] has an APRN ladder now, and we are building our LPN clinical ladder and competency as well. And they are all deeply integrated, so that should someone want to go in that direction, we can make that integration seamless for them,” noted Gabala.
Robust governance ensures data accuracy, security, and compliance, while leadership buy-in drives adoption. Change management strategies must balance results, processes, and relationships, creating psychological safety and empowering teams to innovate.
Africa supported this conclusion by conducting interviews with CNOs across the country, from small rural hospitals to large health systems, finding considerable variation in the level of technological adoption nationwide— the greatest challenge lies in building a robust governance structure around their technology.
“The American Health Information Management Association emphasizes greatly that governance is necessary to ensure that data is accurate, secure, and usable across its life cycle from collection to analysis,” Africa added. “Without governance, the integration efforts risk becoming chaotic and non-compliant. It’s really difficult to just automatically adopt a new technology or adopt AI without knowing what the implications would be— not only for the organization, but for the patients that we care for.”
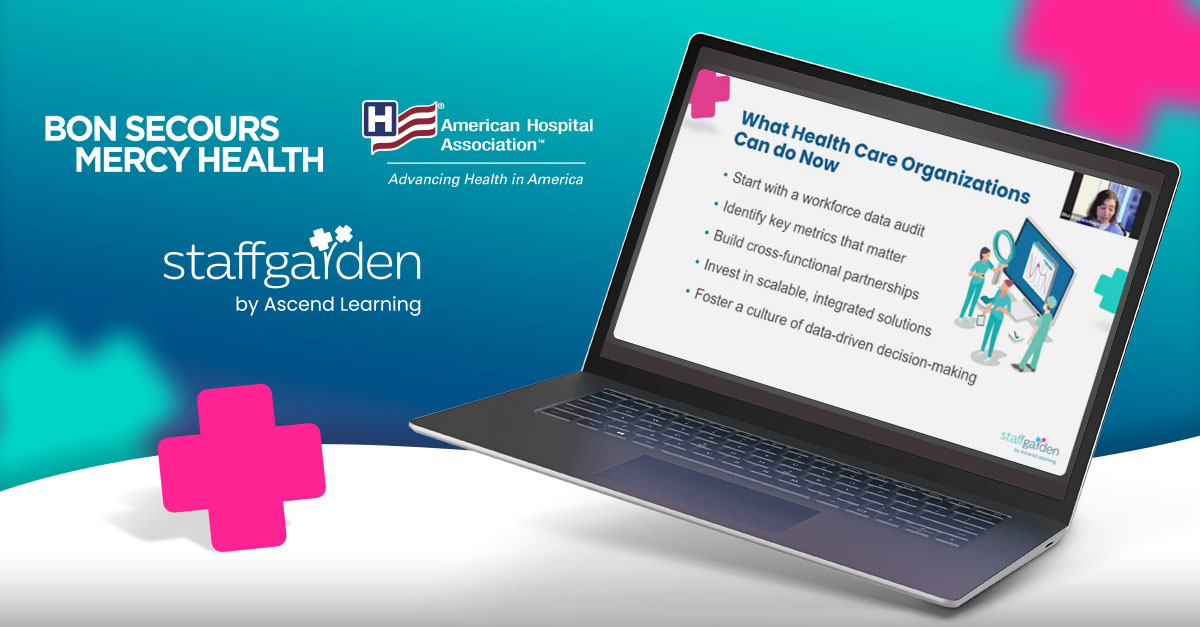
Given the urgency of digital transformation, the panelists outlined practical steps for organizations ready to begin today:
1. Conduct a workforce data audit to identify gaps and validate existing data.
2. Define key metrics that matter for operational and strategic decisions.
3. Build cross-functional partnerships acrossHR, IT, and clinical teams.
4. Invest in scalable, integrated solutions that support real-time insights.
5. Foster a culture of data-driven decision-making to sustain progress.
Starting small by piloting in one market or department allows organizations to refine processes before scaling systemwide.
As a large organization, Bon Secours Mercy Health began by conducting an audit that “revealed that we don’t have confidence in the manual data that we have, or within the systems that we have because it was muddied by so many other confounding factors.”
Going digital has been transformative for Bon Secours MercyHealth because “having bidirectional communication from our systems into [StaffGarden]and back gives us more robust data. We need to be able to tell our story in nursing, and we can’t do that with siloed data points. You need to be able to look at your patient experience in correlation with your competency, and the composition of that staff, to have the right skills meeting the right needs of our patients,” Gabala shared.
Creating a robust, integrated data system is no longer optional. Technology must serve as an enabler, not a distraction. When aligned with strategy, integrated platforms reduce administrative burden, improve patient care, and create meaningful career pathways for healthcare professionals.
The future of healthcare lies in connected, intelligent systems that empower leaders to make proactive decisions and clinicians to deliver safe, competent care. Organizations that embrace this shift will not only survive but thrive in an increasingly complex healthcare landscape.
Watch the full AHA Affinity Forum Session Three recording now.

As a leader in ensuring quality, safety, and efficiency in patient care, your role is vital. Sign up to receive Insights in your inbox and get monthly updates, expert perspectives, and practical information to empower your team and elevate patient care.
Ready for a Modern Approach to Clinical Success?